What do you do if you undergo a big personality change? A personality change can be caused by many causes. It can result from a stressful job, emotional problems, or unhappy relationships. Moreover, your personal changes could be a warning sign of your health problems. If you suddenly notice personality changes, some conditions may be to blame. It’s time for you to discover which conditions cause your personality changes.

Your personality changes can be caused by many reasons
When Does Your Personality Changes Become a Big Problem?
Your personality changes can occur when you have a dramatic change in your life appearance, actions, or emotions. Personality changes seem to be normal in some stages of your life. Because of surrounding factors, your mood changes that lead to your personality changes as well.
However, if your personality changes are uncontrollable, detrimental, and uncomfortable, these can be a big problem. Once experiencing these changes, they signal a deeper problem in your body. You need to see your doctor soon to check.
Related: Could Stress and Low Emotions Cause Your Joint Pain?

If your personality changes are uncontrollable, detrimental, these are a big problem
Which Conditions Cause Your Personality Changes?
There’re many factors contribute to your personality changes, including health conditions. Take a look at the following conditions that can cause your personality changes.
-
Alzheimer’s Disease
This is one of the common conditions cause your personality changes. It has an impact on your thoughts, judgment, and decision- making. Besides, it makes you confused and changes your actions. In the early stage, you will be more anxious and easily annoyed. Then, this disease affects your health seriously. A thoughtful and sweet person can become bossy, or you may be worried too much and get stressed easily.
-
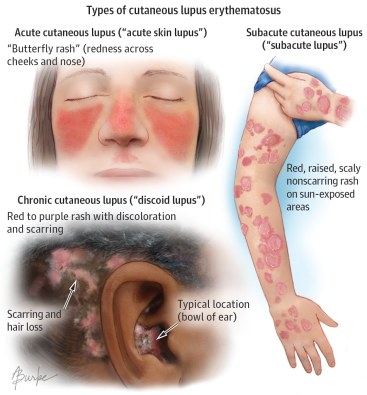
Systemic Lupus Erythematosus (SLE)
Lupus is a complicated autoimmune disease that leads to your personality changes. Because it damages many organs inside your body, people with lupus undergo a number of intense symptoms. Joint pain, fatigue, headaches, or kidney inflammation are what they can tolerate. Once suffering from intense symptoms, lupus patients seem to change their personality. They become hopeless, isolated, depressed, and easily anxious.
If left untreated, lupus can attack many internal organs and progress a life-threating disease. Though lupus is hard to diagnose and treat, making lifestyle changes can help you to deal with this disease. LupuFree, omega-3 fish oil are great supplements to help control lupus symptoms and prevent lupus flare-ups.
Related: 5 Autoimmune Disease Symptoms You Should Never Ignore

Lupus is an autoimmune disease which can cause your personality changes
-
Parkinson’s Disease
Although it only begins as a shakiness in your hands, Parkinson’s disease has an impact on your walking, talking, and thinking over time. In the early stage, you may be obsessed with small details or have carelessness. Then, this disease progresses and makes you absent-minded. As a result, you feel hard to control your thinking in one direction.
In addition, Parkinson’s disease leads to depression and emotional changes, such as fear, anxiety, or hopelessness. Sleep problems can also occur which result in behavior changes.
-
Multiple Sclerosis (MS)
This is also another condition that causes your personality changes. Because once developing multiple sclerosis, your immune system affects the nerves in your brain and spine. Then, it causes many health problems, like bladder issues or movement difficulties. In some cases, MS leads to euphoria feeling where you are beyond happiness. Also, you may experience laughing or crying which is out of control.
This condition can be challenging to diagnose because it can be confused with other diseases. But your doctor will examine your symptoms and give you some tests to diagnose your disease.

Multiple sclerosis causes many health problems, including bladder issues or movement difficulties
-
Thyroid Disease
Thyroid disease is also a condition causes your personality changes. If your thyroid is overworking, it can be put under pressure and affect your personality. You will be more anxious, irritable, and have big mood changes. Over time, thyroid disease progresses into other problems, including forgetfulness or having a hard time to think. If left untreated, it can have a long-lasting effect on your brain.
-
Stroke
Your personality changes can be caused by a stroke. When blood flow reduces, the cells there can’t get enough oxygen and begin to die. This has a serious impact on our body. You may not able to move in some parts of the body. Also, it changes your personality in some ways. For example, you can lose your patience easily and have severe mood swings.
-
Depression
When depression comes, it affects every part of the body and makes your personality changes as well. Not only does depression affect your moods, but it also has an impact on your memory, your thought, and how you make decisions. Once developing depression, you always feel hopeless, sad, guilty, and angry. It’s hard for you to manage your emotions. While women with depression are more likely to feel sad, worthless, and guilty, men tend to feel angry, tired, and irritated.

Depression has a negative impact on your personality changes
Your Personal Changes Can Be Caused By Alcohol and Drug Use
Besides health conditions, your personal changes can be caused by your unhealthy habits. There’s no doubt when drug and alcohol cause your personality changes. These stimulants will make a person manic, lead to depression, or even dementia. Also, some drugs, like heroin, morphine, and opium can result in delirium, dementia, and psychosis changes.
If these cause your personal changes, you should keep them far from your life. You can ask your doctor or relative for help if you’re abused.
There’re many factors in your life lead to your personality changes, including your job and your relationships. Moreover, health conditions have a big impact on your personality changes. Look at the above conditions to raise your awareness if you experience changes in your personality.